CRISPR gene editing is revolutionizing the field of genetic research, opening doors to potential cures for previously debilitating diseases. With this powerful gene editing technology, scientists can now precisely modify DNA sequences, offering hope for conditions like sickle cell anemia. However, the rise of CRISPR also raises significant ethical issues surrounding the implications of altering human genetics. While the benefits of CRISPR are manifold, including the potential for health equity in gene editing access, the associated risks cannot be overlooked. As we delve further into the promise of CRISPR, it becomes crucial to weigh the medical advancements against the moral dilemmas they present.
Gene modification via CRISPR technology has sparked intense discussions among healthcare professionals and ethicists alike. This innovative form of genetic manipulation holds the key to treating an array of genetic disorders, from sickle cell disease to more complex syndromes. Yet, the conversation inevitably veers towards the ethical ramifications of such interventions, including the definition of health equity in gene editing. As we explore the landscape of gene editing techniques, it’s essential to assess both the profound benefits and potential risks these advancements introduce into our society. With each breakthrough, we must also consider who gets to decide the future of genetic health.
Understanding CRISPR and Its Impact on Disease Treatment
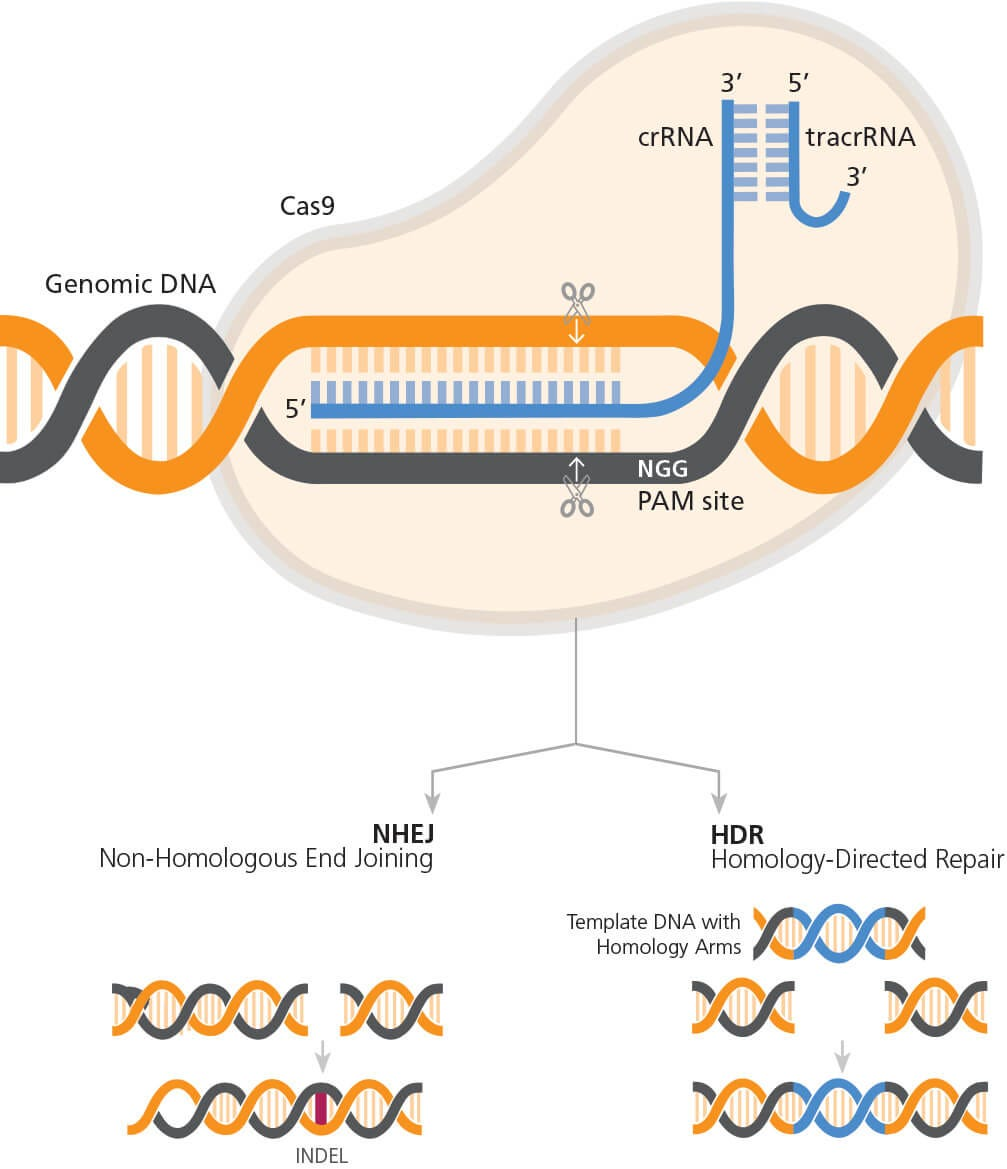
CRISPR gene editing technology has revolutionized the potential for treating various genetic disorders, particularly sickle cell disease. This innovative approach allows scientists to accurately edit genes by removing or altering defective sequences that cause such conditions. With CRISPR, we can manipulate somatic cells to effectively eliminate the symptoms of sickle cell anemia, providing hope to the many individuals impacted by this disorder. Notably, the power of this gene editing technology could also extend to the manipulation of germline genes, potentially eradicating genetic diseases before birth, which sparks a new frontier in medical science.
However, the application of CRISPR raises significant concerns regarding ethical boundaries and health equity. As Neal Baer emphasizes, the discussion is not solely about the efficacy of the treatment but also about who gets access and what implications arise from modifying human genes. With therapies often costing millions, there are pressing questions regarding fairness in healthcare—how do we ensure that advancements benefit everyone and not just the privileged few? As the conversation around CRISPR continues, the need for a thoughtful approach to gene editing technology becomes increasingly critical.
Ethics and Responsibilities in Gene Editing
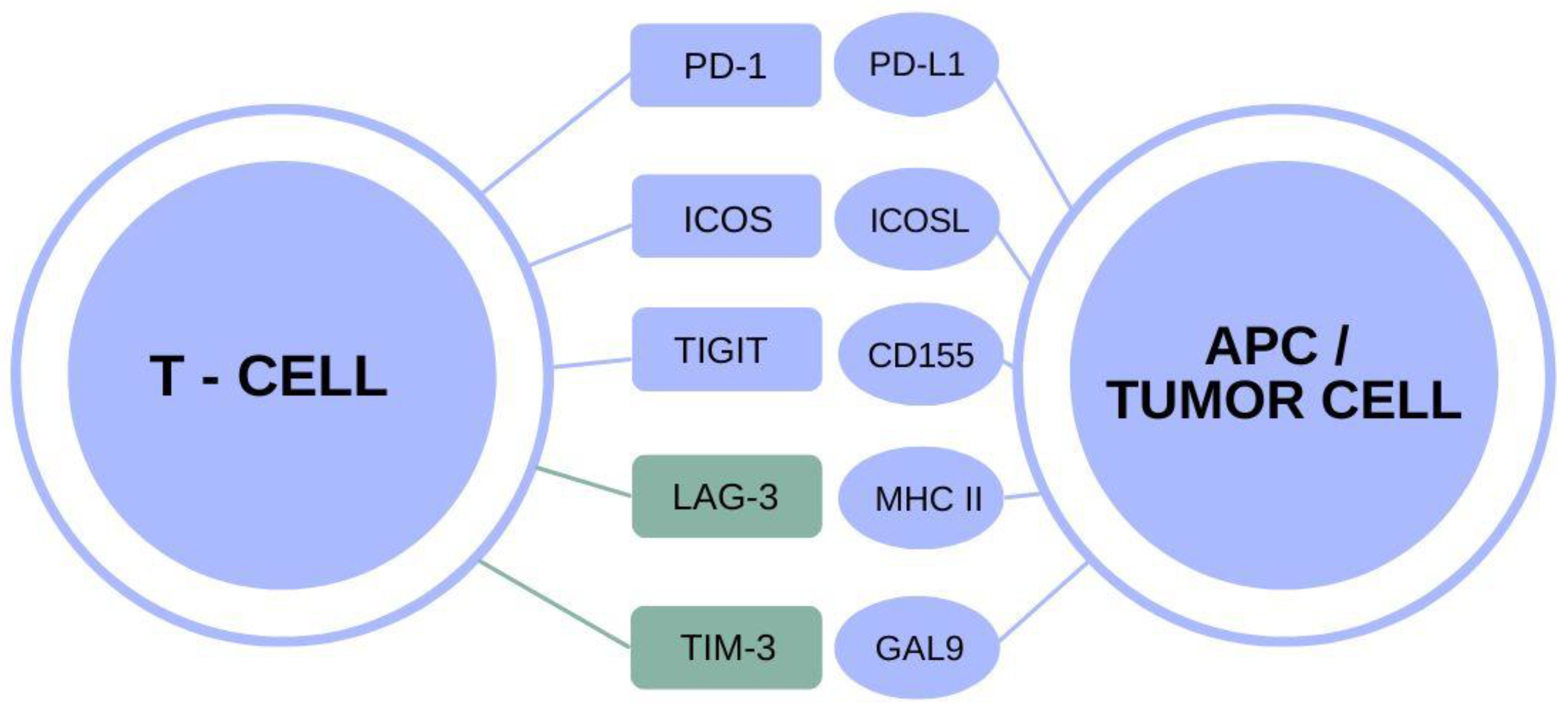
The ethical dilemmas surrounding CRISPR gene editing are complex and multifaceted. One core concern relates to the notion of ‘playing God’—where does the line lie between treatment and enhancement? For instance, should CRISPR be employed to modify traits associated with conditions that are not necessarily life-threatening, such as Down syndrome? This raises profound questions about parental rights and parental decision-making as to the attributes of future children. Furthermore, the discussion around human variation versus pathology challenges us to reconsider societal norms and values.
Additionally, the implications of gene editing extend beyond individual choices to societal responsibilities. As Dr. Rebecca Weintraub Brendel pointed out during the talk, innovation in gene editing technology has the potential to exacerbate existing disparities in healthcare, emphasizing the urgency of addressing health equity. Amidst the excitement of scientific breakthroughs, it is essential to consider the ramifications on marginalized communities who may feel the adverse effects of unequal access to cutting-edge treatments. The ethical discourse must evolve in tandem with technological advancements, promoting justice and fairness in the world of modern medicine.
The Promise and Peril of Sickle Cell Gene Therapy
Sickle cell gene therapy represents a promising application of CRISPR technology, giving hope to individuals suffering from a lifelong condition that significantly affects their quality of life. With the ability to precisely target and edit the genetic factors causing sickle cell anemia, CRISPR has the potential not just to alleviate symptoms, but potentially to cure the disease outright. However, as with any pioneering medical intervention, it carries inherent risks and uncertainties that must be scrutinized carefully.
The cost of the sickle cell treatment, estimated at $2.2 million, poses significant barriers to access for many. This reality underscores the ethical issues regarding who can afford such life-saving therapies and who is left to navigate the challenges posed by genetic disorders without effective treatment options. By examining the potential benefits of sickle cell gene therapy alongside its financial implications, the discourse around CRISPR gene editing must push towards achieving equitable healthcare solutions that ensure all individuals, particularly those in underserved populations, have access to these revolutionary treatments.
As the conversation evolves, the potential of CRISPR technology must be balanced with a commitment to ethical standards and social responsibility, ensuring that we do not leave the most vulnerable behind.
Challenges of Oversight in CRISPR Technology
The rapid advancement of CRISPR gene editing technology poses significant challenges in terms of regulatory oversight. As highlighted by Neal Baer, while legal restrictions may exist in countries like the United States, monitoring practices in other nations, such as China or Russia, can be lax, leading to potentially unsafe applications of gene editing. This raises serious concerns about the global implications of gene editing and the need for an international consensus on ethical standards and safety in genetic research.
The prospect of misuse is further complicated by the increasing commercialization of gene editing technologies. The potential for military or unethical applications, such as creating genetically modified soldiers, exemplifies the dangers that lurk within the unregulated exploration of gene editing. Consequently, the scientific community must advocate for stringent oversight and robust ethical guidelines to prevent misuse of CRISPR technology while ensuring that innovations benefit humanity rather than exploit it.
Health Equity and Access to Gene Therapy
Health equity remains a critical concern as gene editing technologies like CRISPR become more mainstream. The disparity in access to advanced medical treatments highlights a broader issue within the healthcare system, where socioeconomic factors dictate the ability to receive care. As discussed during the Science Center talk, targeting diseases like sickle cell anemia through advanced gene therapies should not only be about technological capability but also about addressing the inequities embedded in health outcomes.
Ensuring equitable access to gene therapy entails more than just the introduction of CRISPR treatments; it requires a dedicated effort to eradicate the barriers faced by vulnerable populations. This means advocating for affordable gene therapies, engaging communities in the conversation about genetic health, and striving for policies that safeguard inclusive access to medical advancements. The discussion on health equity in gene editing underscores the responsibility of researchers, policymakers, and society to work collectively to ensure that the benefits of such transformative technologies are shared universally.
Navigating the Risks and Benefits of CRISPR
CRISPR gene editing technology embodies both remarkable potential and substantial risks. On one hand, the ability to correct genetic defects has ushered in a new era of hope for many genetic disorders, including potentially curable conditions like sickle cell disease. However, these benefits come with the caveat of unforeseen consequences—genetic manipulation can have ripple effects on an individual’s broader genetic makeup, leading to possibly harmful outcomes. As highlighted by experts, the long-term effects of such alterations are still largely unknown, necessitating caution and thorough research before widespread implementation.
Moreover, the ethical implications of CRISPR extend beyond just the scientific community; societal dialogue about gene editing must include diverse perspectives, including voices from those who may be affected by these technologies. The risks associated with gene editing, from unintended genetic mutations to issues of consent and personal autonomy, highlight the need for a comprehensive framework that addresses all aspects of CRISPR’s deployment. As we navigate this complex landscape, the focus should be on fostering responsible innovation that prioritizes safety, ethics, and inclusivity.
Public Perception and CRISPR Technologies
Public perception of CRISPR and gene editing technologies significantly influences their acceptance and application. Many individuals exhibit a mix of enthusiasm and trepidation towards these advancements, often driven by media portrayals, popular culture representations, and anecdotal evidence of outcomes. These perspectives shape how society views genetic interventions, thus affecting funding, regulation, and the overall trajectory of CRISPR research.
To foster a more informed public discourse, it is crucial to educate communities about the science behind CRISPR and its implications for health and society. Open dialogues, workshops, and public forums can serve to bridge the gap between scientific communities and the general public, addressing concerns while highlighting the potential benefits. As the narrative around gene editing evolves, a participatory approach is essential for building trust and ensuring that advancements align with societal values.
The Role of Bioethics in Gene Editing
Bioethics plays a pivotal role in shaping the discourse surrounding CRISPR gene editing technologies. As medical scientists and researchers push the boundaries of genetics, ethical considerations must remain at the forefront of discussions. The collaborative dialogue between bioethicists, medical professionals, and the public helps to navigate the moral complexities associated with gene editing, ensuring that humanity’s best interests are considered.
Incorporating diverse ethical perspectives is key to addressing heated debates surrounding CRISPR’s application, particularly regarding sensitive topics like genetic enhancement or designing babies. The responsibility to engage in ethical oversight is not just relegated to scientists but extends to policymakers and society as a whole. As we advance into a future where gene editing will play an increasingly significant role in healthcare, establishing ethical frameworks will be essential in guiding responsible research and development.
Future Directions for CRISPR Technology
The future of CRISPR gene editing technology holds incredible promise, with ongoing research aimed at refining its precision and expanding its applications in medicine. As scientists continue to explore the potential for treating various diseases, including hereditary disorders, the landscape of healthcare is set to transform dramatically. Moreover, advancements in gene editing techniques could open the door to personalized medicine, tailoring treatments to individuals’ unique genetic profiles for more effective outcomes.
However, as we look towards the future, it is imperative to remain vigilant about the ethical and societal implications that accompany such advancements. By fostering interdisciplinary collaborations among scientists, ethicists, policymakers, and the public, we can ensure that the trajectory of CRISPR technology is guided by values that enhance the well-being of all individuals. Building a robust infrastructure for responsible research, public engagement, and equitable access to innovations will be some of the defining challenges as we navigate the next frontier in gene editing.
Frequently Asked Questions
What are the ethical issues surrounding CRISPR gene editing?
CRISPR gene editing raises several ethical issues, including the potential for genetic discrimination, the implications of ‘designer babies,’ and the moral responsibilities of altering human genes. Discussions often center on whether it is appropriate to edit genes for non-lethal conditions or to enhance human traits, questioning who decides what genetic modifications are acceptable.
How does CRISPR technology relate to sickle cell gene therapy?
CRISPR technology has shown promise in treating sickle cell disease by allowing scientists to edit the genes responsible for this painful condition. By manipulating somatic cells, CRISPR can remove the genes that cause sickle cell anemia, potentially providing a cure for affected individuals, although the high costs and health equity implications remain significant concerns.
What are some potential risks of CRISPR gene editing?
The risks of CRISPR gene editing include unintended genetic alterations, which can lead to unforeseen health issues. Additionally, ethical considerations arise over the potential misuse of CRISPR for non-therapeutic enhancements, and issues of unequal access to gene editing technology that could deepen health disparities.
How does health equity play a role in CRISPR gene editing discussions?
Health equity is a critical aspect of discussions surrounding CRISPR gene editing. As the technology advances, disparities in access to gene editing therapies may widen, particularly for underprivileged communities. Ensuring equitable access is essential to prevent exacerbating existing health inequalities, especially for conditions like sickle cell anemia.
What are the benefits of CRISPR gene editing technology?
The benefits of CRISPR gene editing technology include its potential to cure genetic disorders—such as sickle cell disease—enhance agricultural productivity, and provide insights into gene functions. The precision and efficiency of CRISPR make it a revolutionary tool in both medicine and biotechnology.
How is CRISPR impacting the future of genetic research?
CRISPR is significantly impacting the future of genetic research by enabling precise DNA modifications, facilitating breakthroughs in understanding gene functions, and driving forward potential treatments for various genetic diseases. Its versatility and ease of use promise to accelerate advancements in personalized medicine and therapeutic approaches.
| Key Point | Description |
|---|---|
| Ethical Dilemma | Debates on whether changing human traits is a right or a responsibility. |
| CRISPR Technology | Genetic editing tool capable of modifying somatic and germline genes. |
| Sickle Cell Anemia Cure | CRISPR can cure sickle cell through gene editing, but raises cost and accessibility questions. |
| Equity Concerns | Potential disparity in access to gene editing technologies across different populations. |
| Parental Decisions | Ethical implications of allowing parents to decide genetic attributes for their children. |
| Unintended Consequences | Editing genes may produce unforeseen outcomes due to complex gene interactions. |
| Oversight Issues | Lack of international regulation around gene editing practices in some countries. |
Summary
CRISPR gene editing represents a groundbreaking technology with the potential to cure genetic disorders, but it also raises profound ethical questions. While the ability to amend human DNA offers hope for treating ailments like sickle cell anemia, discussions surrounding its implementation focus on equity, oversight, and the moral implications of altering human traits. As society advances in this domain, it is vital to balance innovation with ethical considerations to ensure fair access and prevent misuse of such powerful tools.