In the realm of pediatric brain cancer AI prediction, groundbreaking advancements are being made that could revolutionize patient care. Recent studies have illustrated how artificial intelligence, particularly in medical imaging, can significantly enhance the accuracy of glioma recurrence prediction. By analyzing multiple brain scans over time, AI tools have outperformed traditional methods, providing a clearer picture of recurrence risks in children with brain tumors. With pediatric oncology increasingly embracing machine learning in medicine, the potential for improved treatment pathways and reduced stress for young patients and their families is palpable. As researchers continue to refine these AI models, they pave the way for a future where early detection and targeted interventions become the norm in managing brain cancer in children.
Exploring the intersection of technology and healthcare, we find a promising frontier in the prediction of brain malignancies in youth through advanced artificial intelligence. The deployment of intelligent systems particularly focuses on assessing the likelihood of tumor recurrence in pediatric patients, using a technique that leverages temporal analysis of medical imaging. This innovative approach enhances the precision of predictions regarding the all-too-possible resurgence of gliomas. As the field of pediatric cancer continues to evolve, integrating machine learning methodologies into routine practice could reshape the standards of care and optimize outcomes significantly. Ultimately, the marriage of AI and medical diagnostics heralds a new era in pediatric oncology, where proactive and data-driven strategies elevate the standards of childhood cancer treatment.
Understanding Pediatric Brain Cancer
Pediatric brain cancer, particularly glioma, is an area of intense research due to its unique challenges and treatment responses in younger patients. Unlike adult brain cancers, which often present with distinct patterns and mutations, brain cancer in children can manifest in various forms with differing prognoses. Early diagnosis and treatment are crucial as many childhood gliomas can be surgically removed and treated effectively, but the risk of recurrence persists, making the role of accurate monitoring essential.
The need for precise evaluation tools has spurred advancements in pediatric oncology, influencing treatment decisions and outcomes significantly. Parents and healthcare providers often face the difficult decision of monitoring for recurrence through regular MRI scans, which can be both time-consuming and anxiety-inducing. Thus, understanding the implications of pediatric brain cancer not only involves the tumor’s biology but also the impact of rigorous monitoring regimes on the quality of life for children and their families.
AI Predictions in Pediatric Oncology
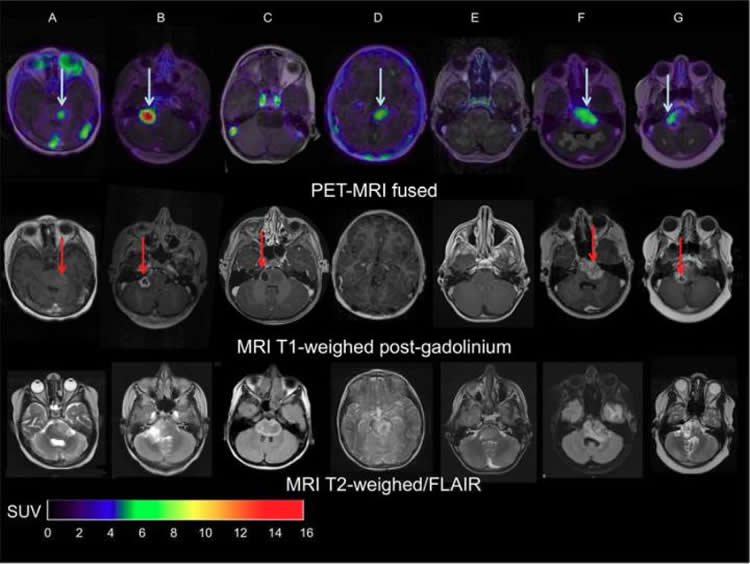
The innovative integration of AI in medical imaging has transformed how we approach pediatric brain cancer. Recent studies have shown that AI tools can predict glioma recurrence significantly better than traditional methods, providing a more efficient way to monitor pediatric patients. By analyzing multiple magnetic resonance imaging (MRI) scans over time, AI can identify subtle changes in brain tumors that may indicate a risk of relapse, ultimately aiding in timely interventions that can save lives.
Machine learning algorithms utilize vast amounts of data to improve their accuracy over time, and this is particularly beneficial in pediatric oncology. By leveraging temporal learning techniques, AI can synthesize data from sequential MRI images, allowing it to predict future tumor behaviors more effectively. This capability not only reduces the burden of frequent imaging on young patients but can also streamline treatment plans, ensuring that care is tailored to the actual risk of recurrence.
The Promise of Temporal Learning
Temporal learning represents a significant advancement in the analysis of pediatric brain cancer. Traditionally, AI models were limited to making predictions based on single imaging sessions, which often resulted in inaccurate assessments of tumor status. However, with temporal learning, researchers have developed models that consider a series of scans taken over time, leading to improved predictive accuracy for glioma recurrence.
The study conducted by Mass General Brigham highlighted the effectiveness of temporal learning, achieving up to 89% accuracy in predicting the recurrence of gliomas. This innovative approach not only enhances diagnostic precision but also holds the potential to optimize treatment strategies. The ability to detect changes in a patient’s brain scans over time allows for better-tailored interventions that could significantly alter patient outcomes in pediatric oncology.
Challenges of Recurrence Prediction
Despite the promising results from AI applications, predicting glioma recurrence remains fraught with challenges. The variability of brain cancers in children means that each case is unique, necessitating highly personalized monitoring approaches. Factors such as tumor type, location, and patient responses to treatment complicate the predictive landscape. Consequently, while AI tools provide significant advancements, they must be viewed as complimentary to clinical assessments rather than standalone solutions.
Moreover, the requirement for extensive datasets to train AI models poses another challenge. Effective training necessitates the aggregation of thousands of images, which may not always be readily available. Consequently, ongoing collaboration between institutions is crucial to gather sufficient data that empowers these AI models to make reliable predictions across diverse clinical settings.
Future Directions in Pediatric Brain Cancer Research
The future of pediatric brain cancer research, particularly in gliomas, looks promising with the incorporation of AI technology. As demonstrated by the recent studies, researchers are hopeful that these AI-driven tools will refine how healthcare providers assess the risk of brain cancer recurrence. This could lead to clinical trials that further evaluate the effectiveness of AI in informing treatment decisions and improving patient outcomes in pediatric oncology.
By blending AI capabilities with traditional medical expertise, there’s potential for advancing treatment paradigms drastically. If AI can successfully predict patient responses and recurrence risks, clinicians can adopt more proactive approaches in managing treatment and monitoring protocols. Ultimately, the goal is to enhance the quality of care provided to young patients while alleviating the emotional and physical burdens associated with frequent diagnostic imaging.
Implementation of AI Tools in Clinical Settings
For AI tools to become integral in pediatric oncology, systematic implementation in clinical settings is essential. This involves not only the validation of AI algorithms across various demographics and hospitals but also the education of healthcare professionals on how to effectively integrate these tools into practice. Medical practitioners must be trained to interpret AI predictions in conjunction with clinical judgment to make well-informed decisions regarding patient care.
Furthermore, establishing guidelines and best practices for deploying AI in managing pediatric brain cancer will greatly enhance its utility. Stakeholders, including hospitals, research institutions, and regulatory bodies, must work collaboratively to outline standards that ensure safety and efficacy. By building robust support systems, the integration of AI can lead to improved patient outcomes and a more streamlined approach to tackling pediatric brain tumors.
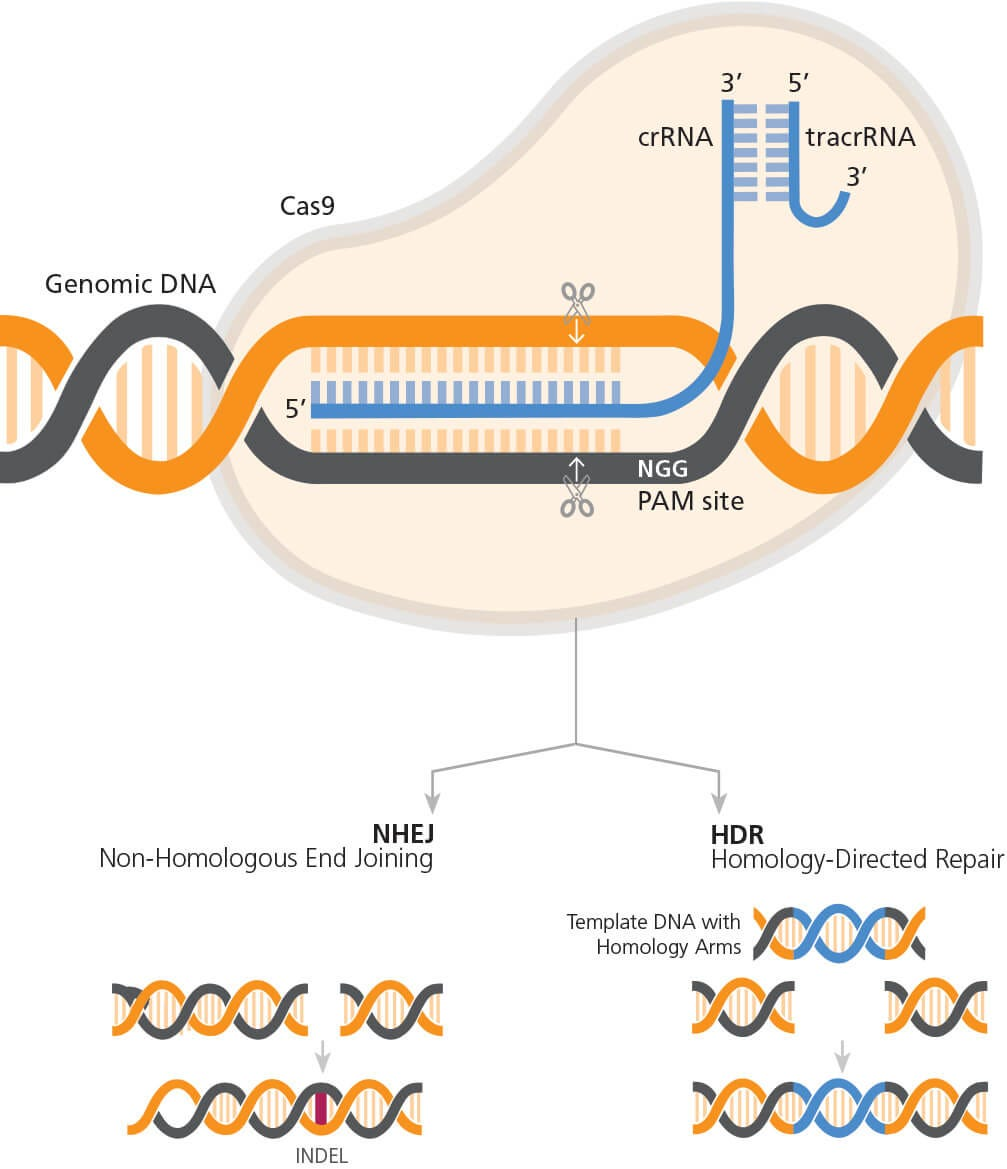
The Role of Machine Learning in Medicine
Machine learning in medicine is reshaping how conditions like pediatric brain cancer are diagnosed and treated. As algorithms become increasingly sophisticated, they can recognize patterns and make predictions that were previously impossible for human clinicians alone. This shift not only enhances the accuracy of diagnoses but also accelerates the pace of research and treatment innovations.
Particularly in pediatric oncology, these advancements are critical. Machine learning can analyze extensive datasets from different patient demographics, identifying trends that inform treatment pathways and improve survival rates. With the advent of AI tools capable of providing accurate predictions for glioma recurrence, the role of machine learning in medicine is poised to revolutionize care for children battling brain cancer.
Impact of AI on Family and Patient Experience
The use of AI-driven predictive tools in pediatric brain cancer management has the potential to significantly improve the experiences of both children and their families. Continuous monitoring through frequent imaging can be a source of anxiety for patients and their parents. By accurately predicting recurrence using AI, healthcare providers may be able to reduce the frequency of these scans for low-risk patients, ultimately alleviating stress and allowing families to focus on the child’s overall well-being.
Moreover, clearer insights into recurrence risk enable families to make informed decisions regarding care and lifestyle adjustments. This empowerment can contribute positively to the emotional and mental health of both children and caregivers. As a result, integrating AI into clinical practice can lead to a holistic approach that prioritizes the patient experience while maintaining rigorous standards of care in pediatric oncology.
Regulatory Considerations for AI in Healthcare
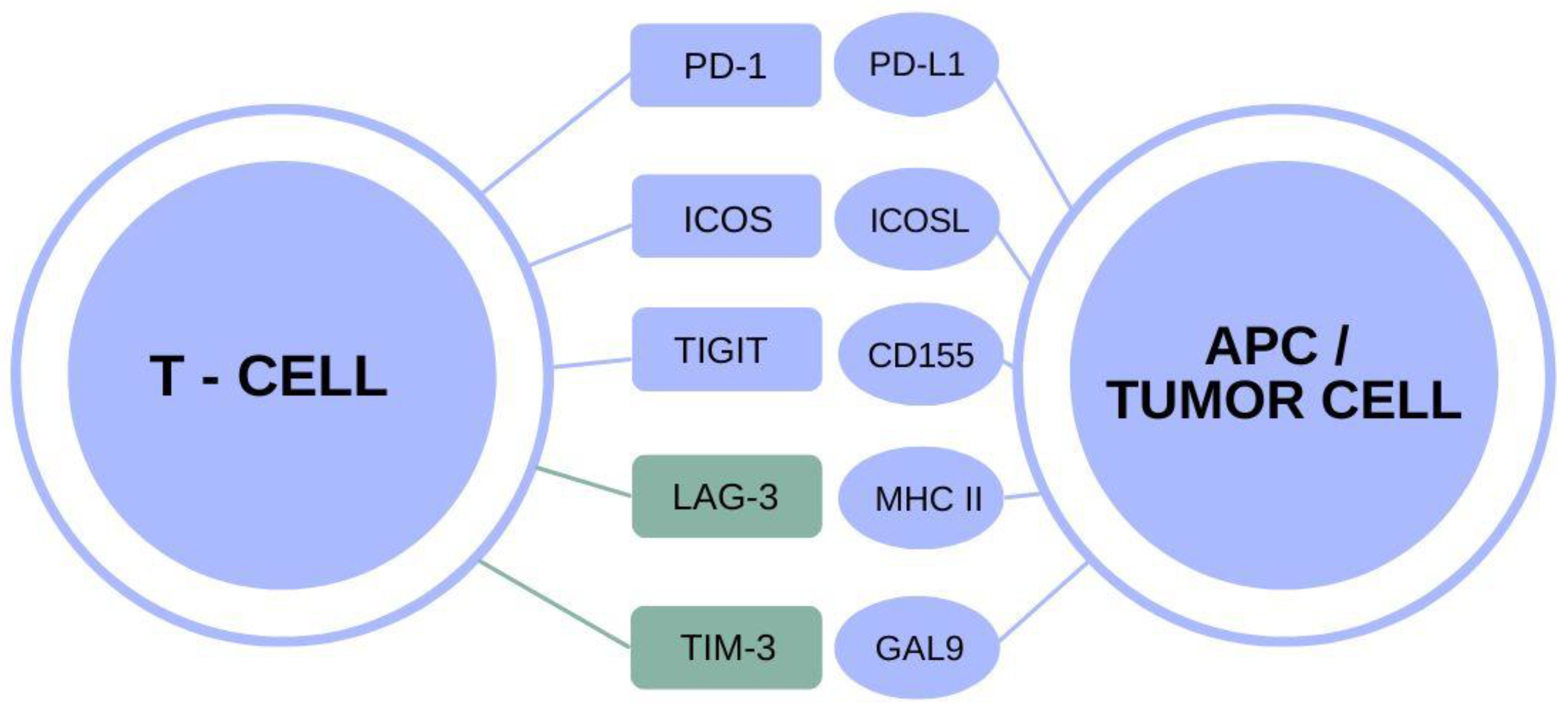
As the integration of AI in predicting glioma recurrence takes root in clinical settings, regulatory considerations will become increasingly important. Ensuring the safety and efficacy of these technologies requires adherence to stringent guidelines posed by healthcare authorities. This involves rigorous testing of AI algorithms and continuous monitoring post-implementation to validate their effectiveness in real-world scenarios.
Additionally, ethical concerns surrounding data privacy and algorithm bias must also be addressed. As AI tools analyze sensitive patient data to make predictions, keeping this information secure and ensuring outcomes are fair and equitable across diverse patient populations is paramount. Regulatory frameworks must evolve in tandem with technological advancements to ensure that AI serves as a beneficial and trusted ally in pediatric oncology.
Frequently Asked Questions
How does pediatric brain cancer AI prediction improve glioma recurrence detection?
Pediatric brain cancer AI prediction leverages advanced algorithms to analyze multiple brain scans over time, enhancing the accuracy of glioma recurrence detection. By employing techniques like temporal learning, AI models can identify subtle changes across successive MRIs, enabling earlier and more precise predictions of potential relapses compared to traditional single-scan methods.
What role does AI in medical imaging play in pediatric oncology?
AI in medical imaging is revolutionizing pediatric oncology by providing accurate predictions for cancer recurrence and treatment outcomes. It processes thousands of MR scans to learn patterns over time, which helps healthcare providers make informed decisions about patient care, ultimately leading to better management of pediatric brain cancer cases.
What advantages does AI offer over traditional methods in predicting brain cancer in children?
AI offers significant advantages in predicting brain cancer in children, including higher accuracy in identifying relapse risks by analyzing multiple imaging timepoints. This contrasts with traditional methods that often rely on individual scans, resulting in a 75-89% prediction accuracy, compared to about 50% for single-image analyses.
How does temporal learning enhance glioma recurrence prediction in pediatric patients?
Temporal learning enhances glioma recurrence prediction by allowing AI models to analyze a sequence of MRI scans taken over time. This method enables the model to capture gradual changes in the tumor environment, thus making more informed predictions about the likelihood of recurrence based on comprehensive data rather than isolated images.
What are the future implications of AI in pediatric brain cancer treatment?
The future implications of AI in pediatric brain cancer treatment include more personalized care strategies, potentially reducing unnecessary follow-up imaging for low-risk patients while ensuring timely intervention for high-risk cases. This could lead to improved patient outcomes and quality of life for children undergoing treatment for brain tumors.
| Key Point | Details |
|---|---|
| AI Predictions | AI tool outperforms traditional methods in predicting relapse risk for pediatric brain cancer patients. |
| Improved Accuracy | The AI model achieved 75-89% accuracy in predicting recurrence compared to 50% accuracy with single image analysis. |
| Temporal Learning | Utilized temporal learning to analyze multiple MR scans over time rather than single images for better predictions. |
| Patient Impact | Enhanced ability to identify patients at risk can potentially ease the stress of MR imaging for children. |
| Future Directions | Clinical trials are planned to test AI-informed risk predictions for improving pediatric brain cancer care. |
Summary
Pediatric brain cancer AI prediction is revolutionizing the way healthcare professionals approach relapse risk assessment in children with gliomas. The use of advanced AI techniques, particularly temporal learning, allows for more precise identification of high-risk patients. By analyzing multiple brain scans over time, this innovative approach not only enhances prediction accuracy but also aims to improve the overall care experience for young patients and their families.